Bilateral Total Cataract in a Young Patient After Septic Shock: Diagnostic and Therapeutic Approach
Main Article Content
Abstract
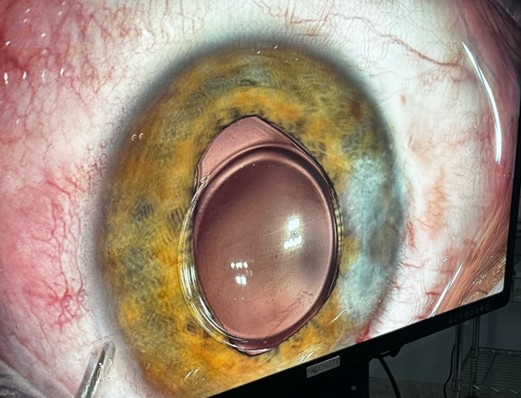
Cataract secondary to severe systemic conditions is a rare but clinically relevant entity, particularly in young patients exposed to intense inflammatory insults such as septic shock. Early identification and timely surgical management can directly impact visual and functional prognosis. To report a case of rapidly progressing bilateral total cataract in a young patient following septic shock, emphasizing clinical presentation, surgical approach, and visual outcomes. This is a qualitative and descriptive case report based on retrospective analysis of medical records, surgical documentation, and ophthalmologic examinations. The patient underwent phacoemulsification with implantation of a monofocal toric intraocular lens in the left eye. Surgery in the right eye is still pending due to financial constraints. The patient demonstrated satisfactory visual recovery in the left eye, with final visual acuity of 20/30. The right eye remains with mature cataract and severely reduced visual acuity. Postoperative follow-up showed good anatomical recovery without complications. This case reinforces the importance of ophthalmologic screening in critically ill patients and highlights that cataract may represent a significant, yet treatable, visual complication following septic shock. Early intervention and the use of advanced intraoperative technologies contribute to favorable visual rehabilitation. Socioeconomic barriers, however, may delay complete visual recovery in vulnerable populations.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors retain the copyright of their articles and grant the journal the right of first publication under the Creative Commons Attribution (CC BY) license, which allows others to share and adapt the work with proper attribution.
References
Boozalis GT, Purdue GF, Hunt JL, McCulley JP. Ocular changes from electrical burn injuries: a literature review and report of cases. J Burn Care Rehabil. 1991;12(5):458–62. doi:10.1097/00004630-199109000-00013.
Saffle JR, Crandall A, Warden GD. Cataracts: a long-term complication of electrical injury. J Trauma. 1985;25(1):17–21. doi:10.1097/00005373-198501000-00004.
Congdon NG, Chang MA, Botelho P, Stark WJ, Datiles MB 3rd. Cataract: Clinical Types. In: Tasman W, Jaeger EA, editors. Duane’s Clinical Ophthalmology. Vol. 1. Philadelphia: Lippincott Williams & Wilkins; 2006. Chapter 73.
Abidi KT, Kamal NM, Bakkar AA, Almarri S, Abdullah R, Alsufyani M, et al. Vici syndrome with pathogenic homozygous EPG5 gene mutation: a case report and literature review. Medicine (Baltimore). 2020;99(43):e22302. doi:10.1097/MD.0000000000022302.
Lee JS, Lee S, Choi M, Lim BC, Choi J, Kim KJ, et al. eIF2B-related multisystem disorder in two sisters with atypical presen-tations. Eur J Paediatr Neurol. 2017;21(2):404–9. doi:10.1016/j.ejpn.2016.07.010.
Betancur JF, Navarro EP, Echeverry A, Moncada PA, Cañas CA, Tobón GJ. Hyperferritinemic syndrome: Still’s disease and catastrophic antiphospholipid syndrome triggered by fulminant Chikungunya infection: a case report of two patients. Clin Rheumatol. 2015;34(11):1989–92. doi:10.1007/s10067-015-3040-9.
Khokhar S, Gupta Y, Rani D, Rathod A, Moharana S. North India Childhood Cataract Study–The real scenario and causes of surgical delay of pediatric cataract. Indian J Ophthalmol. 2022;70(7):2421–5. doi:10.4103/ijo.IJO_293_22.
Tait D. The patient with sepsis and septic shock. In: Acute and Critical Care in Adult Nursing. 1st ed. London: Routledge; 2022. p. 178.
Lin CH, Sun IT. Bilateral simultaneous central retinal vein occlusion secondary to COVID-19: a case report. Case Rep Op-hthalmol. 2023;14(1):56–61. doi:10.1159/000529298.
Ferrara M, Romano V, Longo L, et al. Life-threatening complications in ophthalmic surgery: a systematic review. Eye (Lond). 2025;39(1):69–78. doi:10.1038/s41433-024-03442-1.
Takamatsu K, Kusanagi Y, Horikoshi H, et al. Acute pancreatitis coincided with multiple arteriolar aneurysms in a patient with polyarteritis nodosa. Mod Rheumatol Case Rep. 2022;6(2):234–8. doi:10.1093/mrcr/rxab052.