Juvenile Disseminated Paracoccidioidomycosis in an Immunocompetent Young Patient: A Case Report
Main Article Content
Abstract
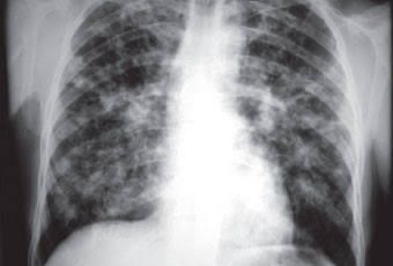
Paracoccidioidomycosis (PCM) is a systemic fungal infection endemic to Latin America, caused by thermally dimorphic fungi of the Paracoccidioides genus. The juvenile form, although less common, presents a diagnostic challenge due to its nonspecific symptoms and frequent absence of pulmonary involvement. We report the case of a 20-year-old male from an endemic region in Brazil who presented with persistent afternoon fever, significant cervical lymphadenopathy, and weight loss. Initial investigations raised suspicion of lymphoma, but histopathological examination of a cervical lymph node biopsy revealed chronic granulomatous lymphadenitis with fungal structures consistent with PCM, confirmed by special stains (Grocott, PAS, and HE). The patient was treated with oral itraconazole 200 mg/day, with favorable clinical response after four weeks. This case underscores the importance of including PCM in the differential diagnosis of prolonged febrile syndromes with lymphadenopathy in endemic areas, highlighting the value of histopathological analysis and early antifungal therapy.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors retain the copyright of their articles and grant the journal the right of first publication under the Creative Commons Attribution (CC BY) license, which allows others to share and adapt the work with proper attribution.
References
Nogueira MGS, Andrade GMQ. Paracoccidioidomycosis in children and adolescents. In: Brazilian Society of Pulmonology and Phthisiology, editor. Pulmonary infectious diseases in children and adolescents. São Paulo: SBPT; 2015. p. 139–49.
Londero AT, Ramos CD, Fischman O. Disseminated “juvenile-type” paracoccidioidomycosis in adolescents: report of four cases and literature review. Arq Bras Med. 1987;61:5–12.
Terra GMF, Gomes LBM, Moreira JLB. Paracoccidioidomycosis in children: case reports. Arq Bras Med. 1991;65:8–15.
De Almeida DC, Santos AP, Oliveira ACR, Lima LN, Xavier TM, Souza PH. Clinical manifestations of paracoccidioidomy-cosis: a literature review. J Arch Health. 2024;5(3):e2028.
Rodrigues PVB, De Andrade Sacramento LM, De Paula TR. Case report of a preschool child with generalized lymphadeno-pathy and diagnosis of paracoccidioidomycosis. Rev Eletr Acervo Saúde. 2024;24:e17954.
Cabral AA, Silva LB, Mendes RAS, Souza JMC, Lopes LGR, Pereira LS, et al. Paracoccidioidomycosis in an immunocompe-tent adolescent: a neglected disease. Rev Med Saúde. 2024;3(2):20–4.
Silva JF, Sousa LE, Lima JC, Macedo CM. Paracoccidioidomycosis: report of 38 cases observed in Teresina (PI). Rev Bras Cir. 1982;72:365–7.
Martinez R, Meneghelli UG, Capuzzo L. Endoscopic evaluation of the involvement of esophagus, stomach, and duodenum in human paracoccidioidomycosis. Arq Gastroenterol. 1986;23(1):21–5.
Moraes-Vasconcelos D, Grumach A, Yamaguti A, Andrade M, Fieschi C, De Beaucoudrey L, et al. Disseminated disease by Paracoccidioides brasiliensis in a patient with inherited IL-12/IL-23 receptor deficiency. Clin Infect Dis. 2005;41(4):e31–7. doi:10.1086/432119.
Diniz R, Silva B, Oliveira Domingues-Da-Silva R, Arnone M, Júnior W, Daher E, et al. Hypercalcemia and acute kidney inju-ry associated with disseminated paracoccidioidomycosis: a case report. Am J Trop Med Hyg. 2024. doi:10.4269/ajtmh.24-0456.
Romitti JP, Barbosa AB, Furlanetto RC. Paracoccidioidomycosis. Rev Matogross Odontol Saúde. 2024;3(1):43–61.
Batista JRM, Ferreira MLR, Oliveira JG, Santana KGM, Rocha JF, Silva BB. Juvenile paracoccidioidomycosis presenting with generalized lymphadenopathy: a diagnostic challenge. Braz J Infect Dis. 2023;27(1):41–4.
Oliveira VMS, Farias RVS, Sousa RMS, Costa KRC, Lopes MHB. Unusual presentation of acute paracoccidioidomycosis in adolescence: case report and literature review. Rev Inst Med Trop São Paulo. 2023;65:e18. doi:10.1590/S1678-9946202365018.
Marinho ÉPA, da Silva VM, Pereira LA, Santos JC, Nogueira Neto JF. Juvenile paracoccidioidomycosis in a rural worker from Central Brazil: diagnostic delay and clinical evolution. J Trop Mycol. 2023;4(2):112–9.
Ministério da Saúde (BR). Guia de Vigilância em Saúde: volume 3 – doenças endêmicas. Brasília: MS; 2023.
Queiroz-Telles F, de Hoog S, Santos DWCL, Salgado CG, Vicente VA, Bonifaz A, et al. Paracoccidioidomycosis: current perspectives of a neglected tropical mycosis. Clin Microbiol Rev. 2017;30(1):231–308. doi:10.1128/CMR.00061-16.
Ferreira MS. Paracoccidioidomycosis in immunocompetent and immunocompromised hosts. Curr Fungal Infect Rep. 2013;7(3):220–8. doi:10.1007/s12281-013-0153-z.
Teles FR, Martins VT, Lanza DC, Moreira AP. Paracoccidioidomycosis mimicking lymphoma: a case series. Rev Inst Med Trop São Paulo. 2020;62:e22. doi:10.1590/S1678-9946202062022.
Shikanai-Yasuda MA, Mendes RP, Colombo AL, Queiroz-Telles F, Kono A, Paniago AM, et al. Brazilian guidelines for the clinical management of paracoccidioidomycosis. Rev Soc Bras Med Trop. 2017;50(5):715–40. doi:10.1590/0037-8682-0245-2017.
Assis EF, Batista AC, Araujo AC, Figueiredo AL, Batista FR. Tomographic findings of paracoccidioidomycosis in the abdo-men and thorax. Radiol Bras. 2005;38(4):275–80.
Pereira RM, Jacob CM, Soeiro SM, Yamaguti A, Duarte AJ, Benard G. Pulmonary manifestations in paracoccidioidomycosis: high-resolution computed tomography study. Rev Inst Med Trop São Paulo. 2004;46(4):185–90.
De Brito AC, Arantes TD, Machado PC, Leite RA. Histoplasmosis and paracoccidioidomycosis: clinical and diagnostic challenges. Curr Trop Med Rep. 2022;9(1):10–9. doi:10.1007/s40475-021-00244-5.
Pedroso VS, Queiroz-Telles F. Pathological features of paracoccidioidomycosis in lymph nodes. Mycopathologia. 2010;170(5):303–9. doi:10.1007/s11046-010-9331-3.
Tavares AH, Silva PC, Batista D, Oliveira PC. Identification of Paracoccidioides species by histopathology and special stai-ning. Med Mycol. 2023;61(1):1–8. doi:10.1093/mmy/myac071.
Queiroz-Telles F, Fahal AH, Falci DR, Caceres DH, Chiller T, Pasqualotto AC. Neglected endemic mycoses. Lancet Infect Dis. 2017;17(11):e367–77. doi:10.1016/S1473-3099(17)30306-7.
Almeida JN Jr, Peçanha-Pietrobom PM, Salomão R. Updates in the treatment of systemic endemic mycoses. J Fungi. 2021;7(8):642. doi:10.3390/jof7080642.