Spontaneous Cholecystocutaneous Fistula: A Case Report
Main Article Content
Abstract
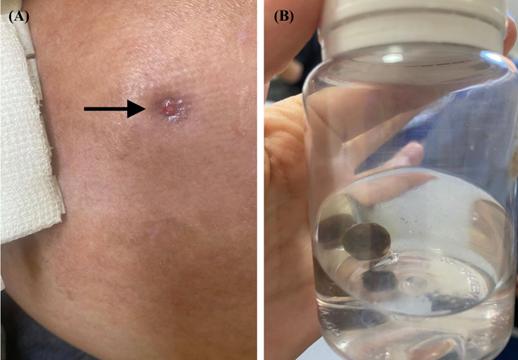
Cholecystocutaneous fistula (CCF) is defined as a pathological communication between the gallbladder and/or its ducts directly with the skin. It is a rare complication of chronic calculous cholecystopathy. Its clinical presentation ranges from gastrointestinal symptoms such as nausea and vomiting, abdominal pain, jaundice, and acute pancreatitis to the drainage of biliary secretion and gallstones through the abdominal wall. The mainstay of treatment involves surgical reconstruction of the biliary anatomy. The incidence of new CCF cases appears to be decreasing due to earlier medical intervention and definitive treatments. This case report presents a patient with acute-on-chronic calculous cholecystitis who developed a CCF with externalization of a gallstone, requiring surgical management.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors retain the copyright of their articles and grant the journal the right of first publication under the Creative Commons Attribution (CC BY) license, which allows others to share and adapt the work with proper attribution.
References
Suárez EB, Navarro-Tovar F, Díaz-Barrientos CZ, Marín-Pardo EI, Hernández-Pérez E. Cholecystocutaneous fistula, an un-common pathology today. Revista de Gastroenterología de México (English Edition) [Internet]. 2023 Apr;88(2):177–9.
Alsaman MZB, Mazketly M, Ziadeh M, Aleter O, Ghazal A. Cholecystocutaneous fistula incidence, Etiology, Clinical Mani-festations, Diagnosis and treatment. A literature review. Annals of Medicine and Surgery. 2020 Nov;59:180–5.
Lofgren DH, Vasani MD S, Singzon MD V. Abdominal Wall Abscess Secondary to Cholecystocutaneous Fistula via Percu-taneous Cholecystostomy Tract. Cureus. 2019 Apr 12;11(4).
Sayed L, Sangal S, Finch G. Spontaneous Cholecystocutaneous Fistula: A Rare Presentation of Gallstones. Journal of Surgical Case Reports. 2010 Jul 1;2010(5):5–5.
Lyon C, Clark DC. Diagnosis of Acute Abdominal Pain in Older Patients. American Family Physician [Internet]. 2006 Nov 1;74(9):1537–44. Available from: https://www.aafp.org/pubs/afp/issues/2006/1101/p1537.html
Guardado-Bermúdez F, Aguilar-Jaimes A, Ardisson-Zamora FJ, Guerrero-Silva LA, Estefanie Villanueva-Rodríguez, Alondra N. Fístula colecistocutánea espontánea. Cirugía y Cirujanos. 2015 Jan 1;83(1):61–4.
Pol MM, Vyas S, Singh P, Rathore YS. Spontaneous cholecystocutaneous fistula: empirically treated for a missed diagnosis, managed by laparoscopy. BMJ Case Reports. 2019 Feb;12(2):e228138.
Malik AH, Nadeem M, Ockrim J. Complete laparoscopic management of cholecystocutaneous fistula. The Ulster Medical Journal [Internet]. 2007 Sep;76(3):166. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC2075592/
Behrend A, Cullen ML. Cholecystocholedochal fistula, an unusual form of internal biliary fistula. Annals of surgery [Internet]. 1950 Aug;132(2):297–303. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1616562/
Birch BRP, Cox SJ. Spontaneous external biliary fistula uncomplicated by gallstones. Postgraduate Medical Journal. 1991 Apr 1;67(786):391–2.
Poudel R. Spontaneous Cholecystocutaneous Fistula: A Case Report. ResearchGate [Internet]. 2015 Apr 17;12(01):51–4. Available from: https://www.researchgate.net/publication/316276975_Spontaneous_Cholecystocutaneous_Fistula_A_Case_Report
Sulakshane S, Thakare V, Dumbre R. Consequences of gallbladder inflammation: spontaneous cholecystocutaneous fistula: a case report. International Surgery Journal. 2018 Apr 21;5(5):1974.
Rinzivillo NMA, Danna R, Leanza V, Lodato M, Marchese S, Basile F, Zanghì GN. Case Report: Spontaneous cholecystocu-taneous fistula, a rare cholethiasis complication. F1000Research [Internet]. 2017 Sep 27 ;6:1768. Available from: https://f1000research.com/articles/6-1768/v1
Tinay OE, Zaka, Mogbil Alhedaithy, Mohamad. Right hypochondrial abscess: A rare consequence of supportive cholecystitis. Annals of Medicine and Surgery. 2016 Nov 25;12:106–8.
Flora HS, Bhattacharya S. Spontaneous cholecystocutaneous fistula. HPB. 2001 Dec;3(4):279–80.
Abbey R: Spontaneous cholecystocutaneous fistula. Int J Adv Integ Med Sci. 2016, 1:196-198.
Nicholson T, Born MW, Garber E: Spontaneous cholecystocutaneous fistula presenting in the gluteal region. J Clin Gastro-enterol. 1999, 28:276-277.
Pripotnev S, Petrakos A: Cholecystocutaneous fistula after percutaneous gallbladder drainage. Case Rep Gastroenterol. 2014, 8:119-122. 10.1159/000362360
Natesan K: A rare complication of a common disease - anterior abdominal wall abscess due to spontaneous rupture of gall bladder. University Journal of Surgery and Surgical Specialities. 2017, 3:99-102. http://ejournal-tnmgrmu.ac.in/index.php/surgery/article/view/4108.
Ongso Y, Beh HN: Cholecystocutaneous abscess: a rare presentation of a common problem. Clin Med Insights Gastroenterol. 2017, 8:44-45. 10.4081/gi.2017.6899
Chopra S, Dodd III GD, Mumbower AL, et al.: Treatment of acute cholecystitis in non-critically ill patients at high surgical risk. AJR Am J Roentgenol. 2001, 176:1025-1031. 10.2214/ajr.176.4.1761025
Davis CA, Landercasper J, Gundersen LH, Lambert PJ: Effective use of percutaneous cholecystostomy in high-risk surgical patients techniques, tube management, and results. Arch Surg. 1999, 134:727-732. 10.1001/archsurg.134.7.727
Malik AH, Nadeem M, Ockrim J: Complete laparoscopic management of cholecystocutaneous fistula. Ulster Med J. 2007, 76:166-167.
Almotlaq AM: Laparoscopic management of a cholecystocutaneous fistula: a case report. J Minim Invasive Surg Sci. 2015, 4:1-3.