Efficacy of Plasma Exchange in Myasthenia Gravis Following Long COVID in a Resource-Limited Context: A Case Report
Main Article Content
Abstract
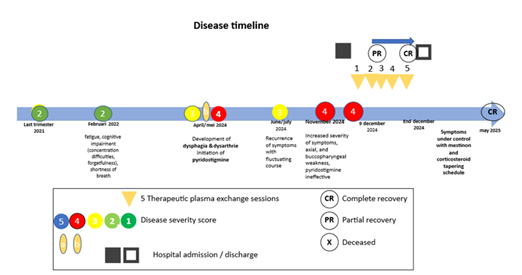
This case report describes the development of myasthenia gravis (MG) in a 71-year-old male patient with long COVID and outlines the management of an MG exacerbation. The patient exhibited significant symptoms, including fatigue, cognitive impairment, dysphagia and dysarthria. Although transient improvement was observed after treatment with pyridostigmine, the patient's condition later worsened, with marked axial and buccopharyngeal weakness. Symptom relief was finally achieved with plasmapheresis using a low-volume crossflow gravity-driven method. This case highlights the potential long-term impact of COVID-19 on autoimmune disorders such as MG and emphasizes the need for vigilance in managing post-COVID neurological complications.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors retain the copyright of their articles and grant the journal the right of first publication under the Creative Commons Attribution (CC BY) license, which allows others to share and adapt the work with proper attribution.
References
Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, Stevens JS, et al. Post-acute COVID-19 syndrome. Nat Med. 2021 Apr;27(4):601-615. doi: 10.1038/s41591-021-01283-z.
Gilhus NE, Tzartos S. Bulbar symptoms and long-term prognosis in myasthenia gravis. Nat Rev Neurol. 2019 May;15(5):287-299. doi: 10.1038/s41582-019-0195-2.
Sanders DB, Wolfe GI, Benatar M, Evoli A, Gilhus NE, Illa I, et al. International consensus guidance for management of myasthenia gravis: Executive summary. Neurology. 2016 Jul 26;87(4):419-425. doi: 10.1212/WNL.0000000000002790.
Tugasworo D, Kurnianto A, Retnaningsih D, et al. The relationship between myasthenia gravis and COVID-19: A systematic review. Egypt J Neurol Psychiatr Neurosurg. 2022;58:83. doi: 10.1186/s41983-022-00516-3.
Bihariesingh-Sanchit R, Bansie R, Sam STA, Lieveld C, Simons A, Kromosoeto J, et al. Gravity-driven crossflow membrane filtration and mechanical centrifugation yield plasma with equivalent total and COVID-19-specific immunoglobulin content. World J Adv Res Rev. 2024;21(2):1107-1115. doi: 10.30574/wjarr.2024.21.2.0527.
Khatri BO, Raval JS. When and how to use plasma exchange therapy for difficult-to-treat multiple sclerosis patients. Inte-chOpen [Internet]. 2025 May 7 [cited 2025 Jun 7]; Available from: https://www.intechopen.com/online-first/1216614. doi: 10.5772/intechopen.1010410.
Restivo DA, Mazzone ME, Marchese-Ragona R, Centonze D, Alesina A. Myasthenia gravis associated with SARS-CoV-2 infection: A case report and review of the literature. J Neurol. 2022 Jan;269(1):45-48. doi: 10.1007/s00415-021-10785-2.
Sriwastava S, Shrestha AK, Khalid SH, Tandon M, Kataria S, Daimee M, et al. New-onset myasthenia gravis after SARS-CoV-2 infection: Case report and literature review. BMJ Case Rep. 2021 Sep;14(9):e244146. doi: 10.1136/bcr-2021-244146.
Dalakas MC. Autoimmune neurological syndromes triggered by COVID-19: A systematic review. Nat Rev Neurol. 2021 Mar;17(3):143-154. doi: 10.1038/s41582-020-00444-9.
Jacob S, Kapadia R, Soule T, Luo H, Schellenberg KL, Douville RN, et al. Neuromuscular complications of SARS-CoV-2 and other viral infections. Front Neurol. 2022;13:914411. doi: 10.3389/fneur.2022.914411.
Bihariesingh-Sanchit R, Bansie R, Ramdhani N, Mangroo R, Bustamente D, Diaz E, et al. Reduced mortality among COVID-19 ICU patients after treatment with HemoClear convalescent plasma in Suriname. mBio. 2023 Mar;14(2):e03379-22. doi: 10.1128/mbio.03379-22.
Jiang X, et al. Myasthenia gravis exacerbation and myasthenic crisis associated with COVID-19: Case series and literature review. J Neurol. 2020. doi: 10.1007/s10072-021-05823-w.
Roca E, et al. The relationship between myasthenia gravis and COVID-19: A systematic review. Egypt J Neurol Psychiatr Neurosurg. 2021. doi: 10.1186/s41983-022-00516-3.