Oral Lesions as the First Clinical Sign of Multifocal Paracoccidioidomycosis: A Case Report
Main Article Content
Abstract
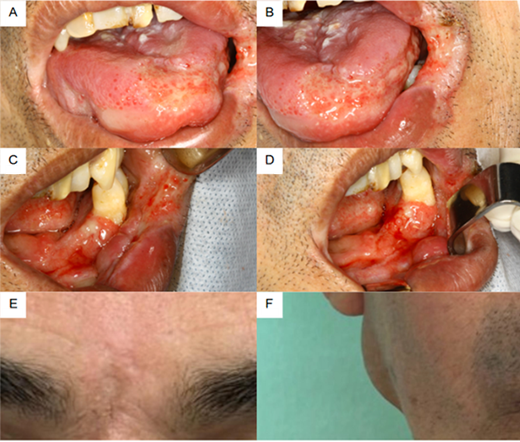
To report a multifocal case of paracoccidioidomycosis (PCM) with oral, pulmonary, and adrenal involvement, highlighting diagnostic challenges and the role of dental professionals in early detection. A 50-year-old Brazilian man, smoker, and alcohol user presented with oral ulcers, weight loss, and respiratory symptoms. Clinical, histopathological, and imaging analyses confirmed PCM by Paracoccidioides brasiliensis with pulmonary and adrenal dissemination. Treatment included liposomal amphotericin B, hydrocortisone replacement, and photodynamic therapy (PDT) for oral lesions, followed by sulfamethoxazole-trimethoprim maintenance. Combined therapy led to resolution of oral and cutaneous lesions, respiratory improvement, and adrenal stabilization. After 10 months, the patient showed weight gain and no recurrence. Despite Brazil’s high PCM prevalence, delayed diagnosis remains common due to non-mandatory reporting and limited professional awareness. Oral manifestations preceded systemic symptoms, emphasizing the dentist’s role in early diagnosis. PCM is an underdiagnosed systemic mycosis with potentially severe outcomes. Recognition of oral lesions as early indicators enables timely intervention and prevents systemic complications. Strengthening awareness among dental and medical professionals, along with improved epidemiological surveillance, is essential to enhance prognosis and reduce morbidity.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors retain the copyright of their articles and grant the journal the right of first publication under the Creative Commons Attribution (CC BY) license, which allows others to share and adapt the work with proper attribution.
References
Griffiths J, Colombo AL, Denning DW. The case for paracoccidioidomycosis to be accepted as a neglected tropical (fungal) disease. PLoS Negl Trop Dis. 2019;13(5): e0007195.
Hotez PJ, Fenwick A, Savioli L, Molyneux DH. Rescuing the bottom billion through control of neglected tropical diseases. Lancet. 2009;373(9674):1570–5.
Ministério da Saúde (BR). Guia de vigilância em saúde. 5a ed. Brasília: Ministério da Saúde; 2019.
Canteros CE. Paracoccidioidomicosis: crónica de una enfermedad olvidada. Rev Argent Microbiol. 2018;50(3):180–4.
Barrozo LV, Benard G, Silva ME, Bagagli E, Marques SA, Mendes RP, et al. First description of a cluster of acute/subacute paracoccidioidomycosis cases and its association with a climatic anomaly. PLoS Negl Trop Dis. 2010;4(3):e643.
Albuquerque Neto AD, Amorim Júnior DS, Carvalho YR, Germano AR, da Silva MCP, Germano JMF. Diagnosis and treatment of paracoccidioidomycosis in the maxillofacial region: a report of 5 cases. Case Rep Otolaryngol. 2018;2018:1–6.
Arruda JAA, Monteiro BV, Oliveira LCS, Leão JC, Mesquita RA, Lima JS, et al. A multicentre study of oral paracoccidioi-domycosis: analysis of 320 cases and literature review. Oral Dis. 2018;24(8):1492–502.
Costa A, de Souza BC, Vilela A, da Silva J, Sousa D. A Brazilian male with typical oral and pulmonary paracoccidioidomycosis. Med J Islam Repub Iran. 2019;33:42.
Shikanai-Yasuda MA, Benard G, Martinez R, Almeida DR, et al. Brazilian guidelines for the clinical management of para-coccidioidomycosis. Rev Soc Bras Med Trop. 2017;50(5):715–40.
Martinez R. New trends in paracoccidioidomycosis epidemiology. J Fungi (Basel). 2017;3(1):1.
Rodrigues FB, Machado AA, Martinez R, et al. Paracoccidioidomycosis: epidemiological features of a 1,000-case series from a hyperendemic area in southeast Brazil. Am J Trop Med Hyg. 2011;85(3):546–50.
Ajello L, Polonelli L. Imported paracoccidioidomycosis: a public health problem in non-endemic areas. Eur J Epidemiol. 1985;1(3):160–5.
Lambertucci JR, Botelho JS, Melo FH. Osteomielite pelo Paracoccidioides brasiliensis. Rev Soc Bras Med Trop. 2002;35(3):271–2.
Wagner G, Moertl D, Glechner A, et al. Paracoccidioidomycosis diagnosed in Europe: a systematic literature review. J Fungi (Basel). 2021;7(2):157.
Oliveira MS, Brandão TB, Coracin FL, et al. Diagnosis at different stages of paracoccidioidomycosis with oral manifestation: report of two cases. J Mycol Med. 2020;30(4):101022.
do Valle ACF, Costa RLB, Fialho-Monteiro PC. Interpretation and clinical correlation of serologic tests in paracoccidioi-domycosis. Med Mycol. 2001;39(4):373–7.
Albuquerque Neto AD, Amorim Júnior DS, Carvalho YR, Germano AR, da Silva MCP, Germano JMF. Diagnosis and treatment of paracoccidioidomycosis in the maxillofacial region: a report of 5 cases. Case Rep Otolaryngol. 2018;2018:1–6.
Dornela Verli F, Marinho SA, Figueiredo MAZ, Yurgel LS. Perfil clínico-epidemiológico dos pacientes portadores de para-coccidioidomicose no Serviço de Estomatologia do Hospital São Lucas da Pontifícia Universidade Católica do Rio Grande do Sul. Rev Soc Bras Med Trop. 2003;36(1):47–52.
Souza RAL, Costa ALF, Bormann AP, Sanches MH, Capistrano HM, et al. Oral paracoccidioidomycosis in a non-endemic region from Brazil: a short case series. J Clin Exp Dent. 2019;11(10):e865–70.
Abreu e Silva MA, Carvalho YR, Almeida OP. Important aspects of oral paracoccidioidomycosis: a literature review. Mycoses. 2013;56(5):436–43.
Butala CB, Cave RNR, Fyfe J, Coleman PG, Yang GJ, Welburn SC. Impact of COVID-19 on the neglected tropical diseases: a scoping review. Infect Dis Poverty. 2024;13(1):55. doi:10.1186/s40249-024-01223-2.
Dai T, Gupta A, Murray CK, Vrahas MS, Tegos GP, Hamblin MR. Photodynamic therapy for the treatment of fungal infections: current knowledge and future perspectives. Photodiagn Photodyn Ther. 2022;38:102787. doi:10.1016/j.pdpdt.2022.102787.
Agudelo CA, Restrepo A, Molina D, et al. Identification of Paracoccidioides brasiliensis in adrenal gland biopsies of two patients with paracoccidioidomycosis and adrenal insufficiency. Rev Inst Med Trop Sao Paulo. 2009;51(1):45–8.
Torres CM, Sampaio SA, Pereira W, et al. Destructive lesion of the adrenal gland in South American blastomycosis (Lutz disease). Am J Pathol. 1952;28(1):145–55.
Faiçal S, Barbosa R, Vianna MR, et al. Addison’s disease caused by Paracoccidioides brasiliensis: diagnosis by needle aspiration biopsy of the adrenal gland. AJR Am J Roentgenol. 1996;167(2):280–6.
Oñate JM, Tóbon AM, Restrepo A. Insuficiencia suprarenal secundaria a paracoccidioidomicosis. Biomedica. 2002;22(3):280–6.
Salfelder K, Doehnert G, Doehnet HR. Paracoccidioidomycosis: anatomic study with complete autopsies. Virchows Arch A Pathol Anat Histol. 1969;348(1):51–76.
Tendrich M, Furtado GC, Wanke B, et al. Adrenocortical involvement in paracoccidioidomycosis. In: Franco M, Lacaz CS, Restrepo A, Del Negro G, editors. Paracoccidioidomycosis. Boca Raton: CRC Press; 1993. p.303–10.
Yamaga LYI, Benard G, Hironaka FH, et al. The role of gallium-67 scan in defining the extent of disease in an endemic deep mycosis, paracoccidioidomycosis: a predominantly multifocal disease. Eur J Nucl Med Mol Imaging. 2003;30(6):888–94.