Hydrocephalus Due to Neurocysticercosis in the Cerebral Aqueduct: Case Report
Main Article Content
Abstract
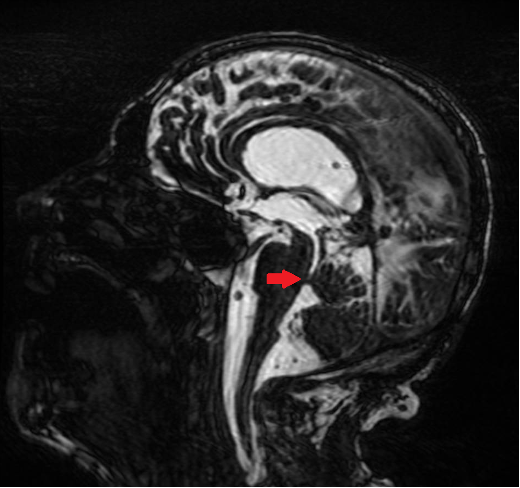
Neurocysticercosis (NCC) is the leading cause of parasitic infection of the central nervous system, resulting from infestation by the larval stage of Taenia solium. Intraventricular forms of the disease, although less frequent, are associated with high morbidity and mortality, mainly due to obstruction of cerebrospinal fluid flow and consequent hydrocephalus. We report the case of a patient previously diagnosed with NCC who presented with acute clinical deterioration secondary to obstruction of the cerebral aqueduct by a cyst compatible with a cysticercus, a location rarely described in the literature. The patient underwent emergency neurosurgical intervention with good clinical outcome. Antiparasitic therapy was not initiated, considering the high number of viable lesions and the risk of an exacerbated inflammatory response. This case report reinforces the importance of early diagnosis of complications associated with NCC, particularly ventricular forms, and expands knowledge of atypical topographic presentations, contributing to improved clinical recognition and appropriate management of the disease.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors retain the copyright of their articles and grant the journal the right of first publication under the Creative Commons Attribution (CC BY) license, which allows others to share and adapt the work with proper attribution.
References
White AC. Neurocysticercosis: Updates on epidemiology, pathogenesis, diagnosis, and Management. Annual Review of Medicine. 2000 Feb;51(1):187–206. doi:10.1146/annurev.med.51.1.187.
Garcia HH, Gonzalez AE, Gilman RH. Taenia solium cysticercosis and its impact in neurological disease. Clinical Microbi-ology Reviews. 2020 Jun 17;33(3). doi:10.1128/cmr.00085-19.
Garcia HH, Nash TE, Del Brutto OH. Clinical symptoms, diagnosis, and treatment of neurocysticercosis. The Lancet Neu-rology. 2014 Dec;13(12):1202–15. doi:10.1016/s1474-4422(14)70094-8.
WHO guidelines on management of Taenia solium neurocysticercosis. Geneva: World Health Organization; 2021.
Coyle CM, Mahanty S, Zunt JR, Wallin MT, Cantey PT, White AC Jr, O'Neal SE, Serpa JA, Southern PM, Wilkins P, McCarthy AE, Higgs ES, Nash TE. Neurocysticercosis: neglected but not forgotten. PLoS Negl Trop Dis. 2012;6(5):e1500. doi: 10.1371/journal.pntd.0001500.
Ndimubanzi PC, Carabin H, Budke CM, Nguyen H, Qian YJ, Rainwater E, Dickey M, Reynolds S, Stoner JA. A systematic review of the frequency of neurocyticercosis with a focus on people with epilepsy. PLoS Negl Trop Dis. 2010 Nov 2;4(11):e870. doi: 10.1371/journal.pntd.0000870.
Del Brutto OH, García HH. Neurocysticercosis in nonendemic countries: time for a reappraisal. Neuroepidemiology. 2012;39(2):145-6. doi: 10.1159/000341693.
Carpio A, Romo ML. State of the art in neurocysticercosis: Imaging and epidemiology. Asian Pac J Trop Med. 2016 Aug;9(8):821-2. doi: 10.1016/j.apjtm.2016.06.010.
Marcin Sierra M, Arroyo M, Cadena Torres M, Ramírez Cruz N, García Hernández F, Taboada D, Galicia Martínez Á, Govezensky T, Sciutto E, Toledo A, Fleury A. Extraparenchymal neurocysticercosis: Demographic, clinicoradiological, and inflammatory features. PLoS Negl Trop Dis. 2017 Jun 9;11(6):e0005646. doi: 10.1371/journal.pntd.0005646.
Bazan R, Hamamoto Filho PT, Luvizutto GJ, Nunes HR, Odashima NS, Dos Santos AC, Elias Júnior J, Zanini MA, Fleury A, Takayanagui OM. Clinical Symptoms, Imaging Features and Cyst Distribution in the Cerebrospinal Fluid Compartments in Patients with Extraparenchymal Neurocysticercosis. PLoS Negl Trop Dis. 2016 Nov 9;10(11):e0005115. doi: 10.1371/journal.pntd.0005115.
Apuzzo ML, Dobkin WR, Zee CS, Chan JC, Giannotta SL, Weiss MH. Surgical considerations in treatment of intraventricular cysticercosis. An analysis of 45 cases. J Neurosurg. 1984 Feb;60(2):400-7. doi: 10.3171/jns.1984.60.2.0400.
Amaral L, Maschietto M, Maschietto R, Cury R, Ferreira NF, Mendonça R, Lima SS. Ununsual manifestations of neurocysti-cercosis in MR imaging: analysis of 172 cases. Arq Neuropsiquiatr. 2003 Sep;61(3A):533-41. doi: 10.1590/s0004-282x2003000400002.
Agapejev S. Aspectos Clínico-Epidemiológicos da neurocisticercose no Brasil: Análise Crítica. Arquivos de Neu-ro-Psiquiatria. 2003 Sept;61(3B):822–8. doi:10.1590/s0004-282x2003000500022
Martins-Melo FR, Ramos AN Jr, Cavalcanti MG, Alencar CH, Heukelbach J. Neurocysticercosis-related mortality in Brazil, 2000-2011: Epidemiology of a neglected neurologic cause of death. Acta Trop. 2016 Jan;153:128-36. doi: 10.1016/j.actatropica.2015.10.011.
Stelzle D, Abraham A, Kaminski M, Schmidt V, De Meijere R, Bustos JA, Garcia HH, Sahu PS, Bobić B, Cretu C, Chiodini P, Dermauw V, Devleesschauwer B, Dorny P, Fonseca A, Gabriël S, Morales MÁG, Laranjo-González M, Hoerauf A, Hunter E, Jambou R, Jurhar-Pavlova M, Reiter-Owona I, Sotiraki S, Trevisan C, Vilhena M, Walker NF, Zammarchi L, Winkler AS. Clinical characteristics and management of neurocysticercosis patients: a retrospective assessment of case reports from Eu-rope. J Travel Med. 2023 Feb 18;30(1):taac102. doi: 10.1093/jtm/taac102.
Nash TE, Ware JM, Mahanty S. Intraventricular Neurocysticercosis: Experience and Long-Term Outcome from a Tertiary Referral Center in the United States. Am J Trop Med Hyg. 2018 Jun;98(6):1755-1762. doi: 10.4269/ajtmh.18-0085.
Riley T, White AC Jr. Management of neurocysticercosis. CNS Drugs. 2003;17(8):577-91. doi: 10.2165/00023210-200317080-00003.