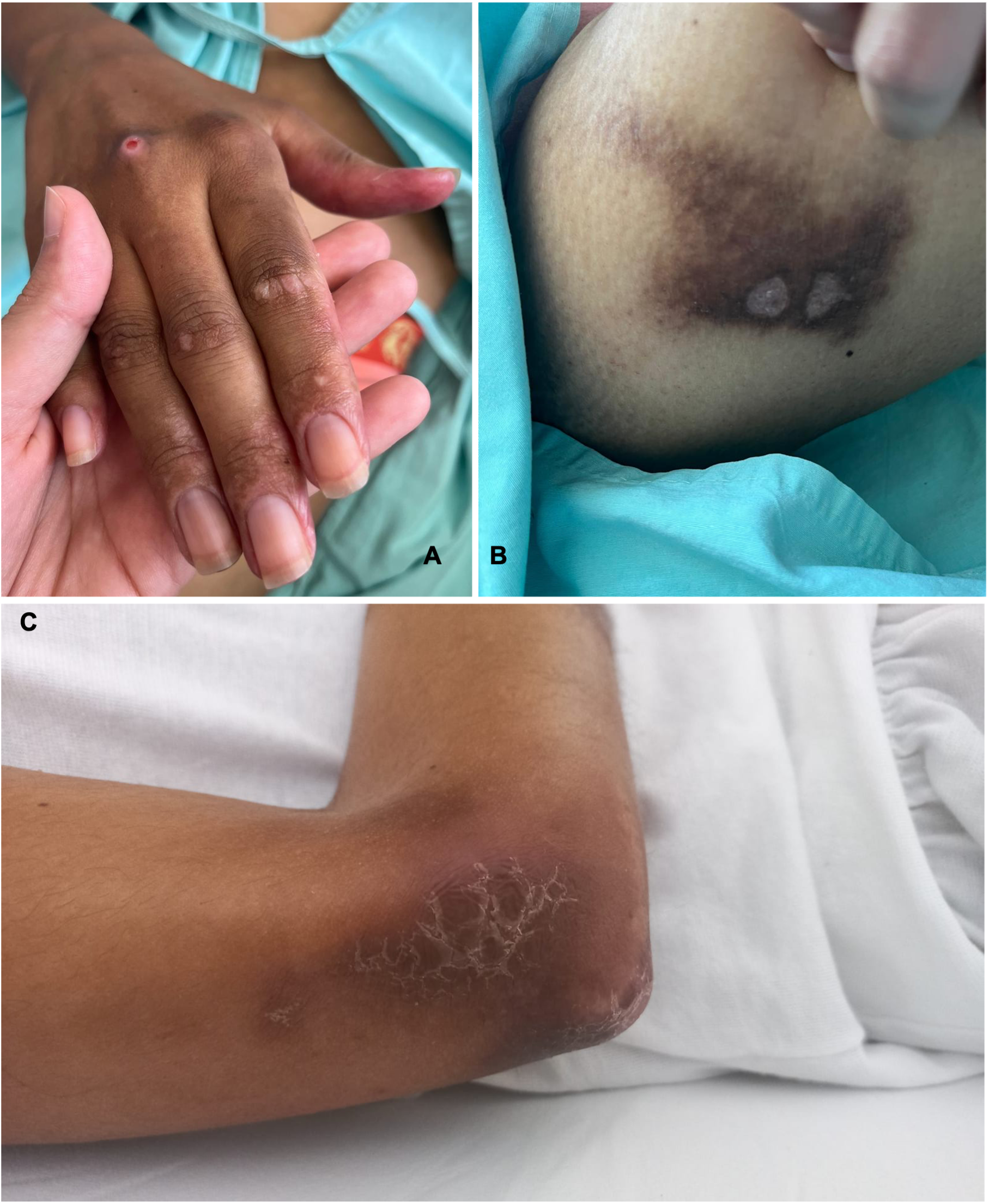
Infecção por Mycobacterium abscessus em Dermatomiosite com Calcinosis Cutis Universalis
Conteúdo do artigo principal
Resumo
Detalhes do artigo

Este trabalho está licenciado sob uma licença Creative Commons Attribution 4.0 International License.
Authors retain the copyright of their articles and grant the journal the right of first publication under the Creative Commons Attribution (CC BY) license, which allows others to share and adapt the work with proper attribution.
Referências
Jiang W, Yang H, Li S, Tian X, Wang G. Clinical features, treatments and outcomes of calcinosis in adult patients with der-matomyositis: a single cohort study. Rheumatology (Oxford). 2021;60(6):2958–62.
Gutierrez A Jr, Wetter DA. Calcinosis cutis in autoimmune connective tissue diseases. Dermatol Ther. 2012;25(2):195–206.
Davuluri S, Duvvuri B, Lood C, Faghihi-Kashani S, Chung L. Calcinosis in dermatomyositis: Origins and possible therapeu-tic avenues. Best Pract Res Clin Rheumatol. 2022;36(2):101768.
Marie I, Hachulla E, Chérin P, Hellot MF, Herson S, Levesque H, et al. Opportunistic infections in polymyositis and derma-tomyositis. Arthritis Rheum. 2005;53(2):155–65.
Haldule S, Chatterjee M, Goswami RP, Vadsaria I, Gaur P, Kavadichanda C, et al. A systematic review and meta-analysis of mycobacterial infections in patients with idiopathic inflammatory myopathies. Rheumatology. 2022;61(9):3521–33.
Huang YC, Liu MF, Shen GH, Lin CF, Kao CC, Liu PY, et al. Clinical outcome of Mycobacterium Abscessus infection and anti-microbial susceptibility testing. J Microbiol Immunol Infect. 2010;43(5):401–6.
Fukui S, Sekiya N, Takizawa Y, Morioka H, Kato H, Aono A, et al. Disseminated Mycobacterium Abscessus infection follo-wing septic arthritis. Medicine (Baltimore). 2015;94(21):e861.
Stout JE, Gadkowski LB, Rath S, Alspaugh JA, Miller MA, Cox GW. Pedicure-associated rapidly growing mycobacterial infection: an endemic disease. Clin Infect Dis. 2011;53(8):787–92.
Gonzales Zamora JA, Villar Astete A. Mycobacterium Abscessus felon complicated with osteomyelitis: not an ordinary nail salon visit. Acta Clin Belg. 2020;75(6):429–33.
Costa-Silva M, César A, Nuno PG, Azavedo F. Mycobacterium Abscessus infection in a spa worker. Acta Dermatovenerol Alp Pannonica Adriat. 2018;27(3):159–60.
Kim J, Kim YJ, Park H, Lee S, Yoo DH. Nontuberculous mycobacterial myositis in dermatomyositis with long-term use of immunosuppressant: a case report. Skeletal Radiol. 2024;53(10):2289–96.
Noguchi S, Hanami K, Miyata H, Torii R, Shimabukuro I, Kubo S, et al. Pleurisy caused by Mycobacterium Abscessus in a young patient with dermatomyositis: a case report and brief review of the literature. Intern Med. 2018;57(7):997–1002.
Spellberg B, Yoo T, Bayer AS. Reversal of linezolid-associated cytopenias, but not peripheral neuropathy, by administration of vitamin B6. J Antimicrob Chemother. 2004;54(4):832–5.