Percutaneous Transhepatic Gallbladder Drainage for Acute Cholecystitis During Chemotherapy: Case Series
Main Article Content
Abstract
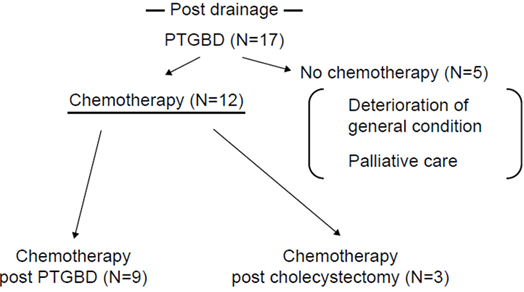
Clinicians may have trouble treating acute cholecystitis in patients undergoing chemotherapy. This study aimed to review the feasibility of continuing chemotherapy while a biliary tube is in place and report our experience. We retrospectively examined the records of 17 patients who underwent percutaneous transhepatic gallbladder drainage (PTGBD) for acute cholecystitis. The cohort comprised nine cases of gastrointestinal cancer and eight other malignancies. Overall, chemotherapy was resumed in 12 cases after PTGBD. These patients were divided into three groups based on the circumstances under which chemotherapy was resumed. Chemotherapy was performed with the drain in place in seven patients (14.33±6.94 days until the start of chemotherapy after drainage, group A), after cholecystectomy in three (84±56 days, group B), and after removing the drainage tube (56 days, group C) in two patients. Early administration of chemotherapy was only possible in group A. At times, clinicians are required to make complicated judgments regarding acute cholecystitis treatment that cannot be done by relying on guidelines alone. With strict control, chemotherapy can be safely resumed, even with a drainage tube in place, and PTGBD can be carefully considered for these patients. These groups were determined retrospectively based on the course of treatment.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors retain the copyright of their articles and grant the journal the right of first publication under the Creative Commons Attribution (CC BY) license, which allows others to share and adapt the work with proper attribution.
References
Gorschlüter M, Mey U, Strehl J, Schepke M, Lamberti C, Sauerbruch T, Glasmacher A. Cholecystitis in neutropenic patients: retrospective study and systematic review. Leuk Res. 2006;30(5):521–8. doi: 10.1016/j.leukres.2005.08.029.
Taplitz RA, Kennedy EB, Bow EJ, Crews J, Gleason C, Hawley DK, Langston AA, Nastoupil LJ, Rajotte M, Rolston K, Strasfeld L, Flowers CR. Outpatient management of fever and neutropenia in adults treated for malignancy: American Society of Clinical Oncology and Infectious Diseases Society of America clinical practice guideline update. J Clin Oncol. 2018;36(14):1443–53. doi: 10.1200/JCO.2017.77.6211.
Agha RA, Borrelli MR, Farwana R, Koshy K, Fowler A, Orgill DP, for the PROCESS Group. The PROCESS 2018 Statement: Updating Consensus Preferred Reporting of Case Series in Surgery (PROCESS) Guidelines. Int J Surg. 2018;60:279–82. doi: 10.1016/j.ijsu.2018.10.031
Okamoto K, Suzuki K, Takada T, Strasberg SM, Asbun HJ, Endo I, Iwashita Y, Hibi T, Pitt HA, Umezawa A, Asai K, Han HS, Hwang TL, Mori Y, Yoon YS, Huang WSW, Belli G, Dervenis C, Yokoe M, Kiriyama S, Itoi T, Jagannath P, Garden OJ, Miura F, Nakamura M, Horiguchi A, Wakabayashi G, Cherqui D, de Santibañes E, Shikata S, Noguchi Y, Ukai T, Higuchi R, Wada K, Honda G, Supe AN, Yoshida M, Mayumi T, Gouma DJ, Deziel DJ, Liau KH, Chen MF, Shibao K, Liu KH, Su CH, Chan ACW, Yoon DS, Choi IS, Jonas E, Chen XP, Fan ST, Ker CG, Giménez ME, Kitano S, Inomata M, Hirata K, Inui K, Sumiyama Y, Yamamoto M. Tokyo Guidelines 2018: flowchart for the management of acute cholecystitis. J Hepatobiliary Pancreat Sci. 2018;25(1):55–72. doi: 10.1002/jhbp.516.
US Department of Health and Human Services, National Institutes of Health – National Cancer Institute. Common Termi-nology Criteria for Adverse Events (CTCAE). version 5. Published: November 27.
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, Carbone PP. Toxicity and response criteria of the eastern cooperative oncology group. Am J Clin Oncol. 1982;5(6):649–55. doi: 10.1097/00000421-198212000-00014.
Miura F, Takada T, Strasberg SM, Solomkin JS, Pitt HA, Gouma DJ, Garden OJ, Büchler MW, Yoshida M, Mayumi T, Okamoto K, Gomi H, Kusachi S, Kiriyama S, Yokoe M, Kimura Y, Higuchi R, Yamashita Y, Windsor JA, Tsuyuguchi T, Gabata T, Itoi T, Hata J, Liau KH, Tokyo Guidelines Revision Comittee. TG13 flowchart for the management of acute cholangitis and cho-lecystitis. J Hepatobiliary Pancreat Sci. 2013;20(1):47–54. doi: 10.1007/s00534-012-0563-1.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83. doi: 10.1016/0021-9681(87)90171-8.
Santos D, Ledet CR, Limmer A, Gibson H, Badgwell B. Use of non-operative treatment and interval cholecystectomy for cholecystitis in patients with cancer. Trauma Surg Acute Care Open. 2020;5(1):e000439. doi: 10.1136/tsaco-2020-000439.
Coccolini F, Improta M, Sartelli M, Rasa K, Sawyer R, Coimbra R, Chiarugi M, Litvin A, Hardcastle T, Forfori F, Vincent JL, Hecker A, Ten Broek R, Bonavina L, Chirica M, Boggi U, Pikoulis E, Di Saverio S, Montravers P, Augustin G, Tartaglia D, Cicuttin E, Cremonini C, Viaggi B, De Simone B, Malbrain M, Shelat VG, Fugazzola P, Ansaloni L, Isik A, Rubio I, Kamal I, Corradi F, Tarasconi A, Gitto S, Podda M, Pikoulis A, Leppaniemi A, Ceresoli M, Romeo O, Moore EE, Demetrashvili Z, Biffl WL, Wani I, Tolonen M, Duane T, Dhingra S, DeAngelis N, Tan E, Abu-Zidan F, Ordonez C, Cui Y, Labricciosa F, Perrone G, Di Marzo F, Peitzman A, Sakakushev B, Sugrue M, Boermeester M, Nunez RM, Gomes CA, Bala M, Kluger Y, Catena F. Acute abdomen in the immunocompromised patient: WSES, SIS-E, WSIS, AAST, and GAIS guidelines. World J Emerg Surg. 2021;16(1):40. doi: 10.1186/s13017-021-00380-1.
Hatanaka T, Itoi T, Ijima M, Matsui A, Kurihara E, Okuno N, Kobatake T, Kakizaki S, Yamada M. Efficacy and safety of en-doscopic gallbladder stenting for acute cholecystitis in patients with concomitant unresectable cancer. Intern Med. 2016;55(11):1411–7. doi: 10.2169/internalmedicine.55.5820.
Mori Y, Itoi T, Baron TH, Takada T, Strasberg SM, Pitt HA, Ukai T, Shikata S, Noguchi Y, Teoh AYB, Kim MH, Asbun HJ, Endo I, Yokoe M, Miura F, Okamoto K, Suzuki K, Umezawa A, Iwashita Y, Hibi T, Wakabayashi G, Han HS, Yoon YS, Choi IS, Hwang TL, Chen MF, Garden OJ, Singh H, Liau KH, Huang WSW, Gouma DJ, Belli G, Dervenis C, de Santibañes E, Giménez ME, Windsor JA, Lau WY, Cherqui D, Jagannath P, Supe AN, Liu KH, Su CH, Deziel DJ, Chen XP, Fan ST, Ker CG, Jonas E, Padbury R, Mukai S, Honda G, Sugioka A, Asai K, Higuchi R, Wada K, Yoshida M, Mayumi T, Hirata K, Sumiyama Y, Inui K, Yamamoto M. Tokyo Guidelines 2018: management strategies for gallbladder drainage in patients with acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci. 2018;25(1):87–95. doi: 10.1002/jhbp.504.
Teoh AYB, Kitano M, Itoi T, Pérez-Miranda M, Ogura T, Chan SM, Serna-Higuera C, Omoto S, Torres-Yuste R, Tsuichiya T, Wong KT, Leung CH, Chiu PWY, Ng EKW, Lau JYW. Endosonography-guided gallbladder drainage versus percutaneous cholecystostomy in very high-risk surgical patients with acute cholecystitis: an international randomised multicentre con-trolled superiority trial (DRAC 1). Gut. 2020;69(6):1085–91. doi: 10.1136/gutjnl-2019-319996.